The prostate gland is a small yet pivotal component of the male reproductive system. Despite its modest size—about that of a walnut—it plays an essential role in fertility and male health throughout life. This review draws on current anatomical and physiological knowledge, supported by medical research, to provide a comprehensive understanding of this organ.
Anatomy and Structural Overview
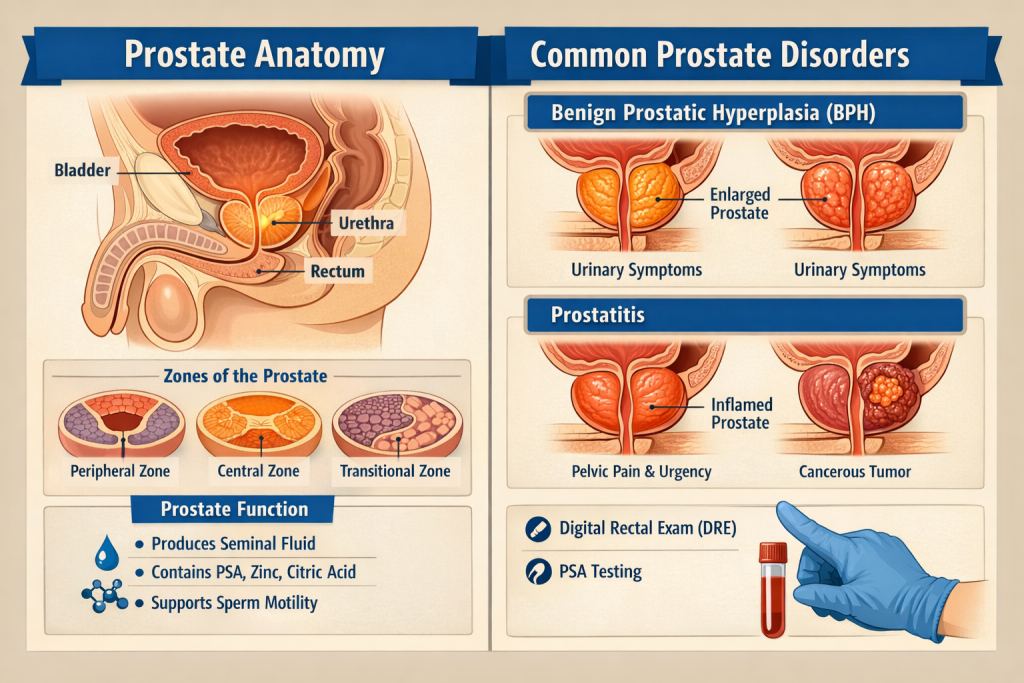
The prostate is situated just below the urinary bladder and in front of the rectum, encircling the urethra—the tube responsible for carrying urine and semen out of the body. Its position means changes in prostate size or texture can impact urination and reproductive function.
Anatomically, the gland is composed of both glandular tissue, which produces secretions, and fibromuscular stroma, which supports structural integrity and function. The prostate is classically divided into regions known as zones—peripheral, central, and transitional—each with distinct clinical relevance (e.g., cancer frequently arises in the peripheral zone).
At the microscopic level, the prostate’s secretory units are tubuloalveolar glands, richly supplied with blood and surrounded by smooth muscle fibers. These muscles are critical for propelling prostatic fluid into the urethra during ejaculation.
Physiology: What the Prostate Does
The primary role of the prostate is to produce and secrete a significant portion of the fluid found in semen. This prostatic fluid is slightly alkaline and contains enzymes like prostate-specific antigen (PSA), fibrinolysin, citric acid, and various ions such as zinc, all of which contribute to sperm viability and mobility. The alkalinity helps counteract the acidic environment of the female reproductive tract, enhancing sperm survival after ejaculation.
In addition to fluid production, the prostate contributes to:
Sperm activation: Prostatic secretions help spermatozoa gain motility.
Ejaculation mechanics: Smooth muscles in the prostate contract rhythmically during climax, aiding semen expulsion.
Hormonal interactions: Androgens, especially testosterone and its more active derivative dihydrotestosterone (DHT), are critical for prostate development and secretory function.
Clinical Importance and Common Conditions
Because of its anatomical location, the prostate is implicated in several common health conditions:
1. Benign Prostatic Hyperplasia (BPH)
As men age, the prostate often enlarges, particularly within the transitional zone. This enlargement can compress the urethra, leading to urinary difficulties such as a weak stream, urgency, and incomplete bladder emptying. BPH is not cancer, but it can significantly impact quality of life.
2. Prostatitis
Inflammation of the prostate—often from bacterial infection or chronic inflammation—can result in pain, urinary symptoms, and discomfort during ejaculation. This condition can affect men of all ages, though it is especially common in younger and middle-aged adults.
3. Prostate Cancer
Prostate cancer is one of the most commonly diagnosed cancers in men globally and a major cause of cancer-related death. Tumors typically originate in the peripheral zone and may be detected via elevated PSA levels or digital rectal examination (DRE), with imaging and biopsy confirming the diagnosis.
Current research continues to refine our understanding of prostate cancer biology. For example, scientists have identified proteins such as TBX-2 and LSD-1 that may contribute to drug resistance in aggressive prostate cancer forms, suggesting potential new therapeutic targets.
Innovations in diagnostics are also emerging. Novel rapid blood tests using advanced imaging of dried blood smears have shown promise for early cancer detection, potentially enhancing screening accuracy beyond traditional PSA measurements.
Hormonal Regulation and Development
The prostate’s growth and function are intricately controlled by steroid hormones. Androgens such as testosterone and DHT are essential for prostate cell differentiation, growth, and secretory activity. Researchers emphasize the importance of cell-cell communication and androgen signaling in maintaining both normal prostate physiology and in the progression of pathological states.
Conclusion
The prostate gland, though small, is a complex and vital organ with roles that extend far beyond fluid production. Its intricate anatomy and physiology are foundational to male reproductive health. As research advances—from molecular studies of hormone regulation to groundbreaking diagnostic tools—our understanding of prostate function and disease continues to evolve, offering hope for improved prevention, diagnosis, and treatment of prostate conditions.
Leave a Reply